
How to write an essay about the middle range nursing theory

Middle range nursing theory is recognized as crucial for the framework of nursing knowledge. An analysis of nine middle range nursing theory, frequently utilized by their creators, is conducted based on their name, development process, disciplinary viewpoint, theoretical framework, application in practice, and research utility.
The critique highlights the significance of long-term engagement with the theory, ensuring its naming and evolution align with the disciplinary view, advancing to an empirical stage, and integrating middle range nursing theory into interdisciplinary discussions.
The role of spirituality in healthcare discussions, particularly in nursing and other health professions within the United States, remains a contentious issue, with ongoing debates about its relevance in patient care and the appropriate methods for its incorporation.
A method proposed for addressing spiritual needs in patient care is through the Framework of Systemic Organization, which serves as a guiding principle for nurses to attend to patients’ spiritual requirements.
Spirituality is characterized by the establishment of connections with entities such as a higher power (God), nature, or other individuals, enabling individuals to find significance in their relationships. Central to providing spiritual care is the creation of a harmonious balance between control and spirituality, customized according to the unique history, values, and necessities of each patient. The article illustrates this approach with a case study demonstrating how a nurse can provide support to a patient confronting end-of-life issues.
List of middle-range theories of nursing:
- Theory of maternal role attainment
- The framework of systemic organization
- Synergy model
- Theory of maternal role attainment
- Nurse as wounded Healer
- Theory of comfort and many
- The theory of unpleasant symptoms
- The theory of self-efficacy
- Theory of empathy
- Theory of pain
- The theory of chronic sorrow
- Theory of social support
- The theory of interpersonal relations
- The theories of reasoned action and planned behavior
- Theory of group power within organizations
- The theory of modeling and role-modeling
- The theory of comfort
- Theory of health-related quality of life
- The theory of health promotion
- The theory of the deliberative nursing process,
- Theory of self-efficacy
- Theory of resilience
- Theories of uncertainly in illness
- Theory of self-efficacy among other middle-range theories.
The Framework of Systemic Organization – Marie-Louise Friedemann (our first middle range nursing theory)
The Framework of Systemic Organization, developed through inductive reasoning by Friedemann, provides a theoretical foundation for the practice of family nursing. This framework has been discussed extensively in academic literature, and its effectiveness in dealing with diverse family types has been proven. Its key aspects of how families function have gained validation via factor analysis of a theory-driven evaluation tool, known as the Assessment of Strategies in Families.
Rooted in the principles of open systems theory and social ecology, this framework offers a universal model for systemic life processes applicable to individuals, families, and broader social entities. It posits that all systems and their sub-systems are part of a greater universal structure and operate in mutual dependence. A diagram, Figure 1, illustrates this systemic process model (in the instance of an individual), highlighting the interconnections among the Framework of Systemic Organization’s primary concepts.
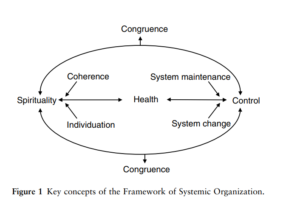
Friedemann suggests that the optimal state for any system is congruence, where the system’s patterns and rhythms are synchronized both internally and with the cosmos. For humans, achieving congruence is akin to reaching a utopian state. Due to constant changes and conflicting values that systems face, striving for congruence is a perpetual endeavor that is never fully realized. The discomfort stemming from this lack of congruence manifests as anxiety. However, humans have the capability to mitigate this tension through their life processes, particularly by finding a balance between controlling their lives and embracing spirituality. The ideal equilibrium varies among individuals, with the preference for control or spirituality influenced by one’s culture, beliefs, and values.
In American society, there’s a strong emphasis on maintaining control, which is understood as the act of modifying any obstacles that disrupt a system’s operation to either restore its original state (homeostasis) or to bring about a minimal disruptive change (morphostasis). This pursuit of control is a defense against our fundamental susceptibility, offering a sense of safety.
To counteract significant disruptive changes, such as serious illness, and to manage anxiety, there’s a concerted effort to revert to previous conditions as much as possible. As depicted on the right side of Figure 1, achieving control involves two key activities – maintaining the system and changing the system.
System maintenance is executed through self-care activities that support the body and mind, addressing physical, psychological, and social requirements. System change involves adopting strategies to adjust to new circumstances, with seeking medical treatment for illness being a primary example of exerting control.
Patients endeavor to fight disease by adhering to medical advice and engaging in strict treatment plans set out by healthcare providers. The goal is to preserve physical health through planned actions and maintenance, while also exerting effort, applying knowledge, and adjusting behaviors to reduce undesired changes (system change). This battle for control occurs at the individual, family, social group, and societal levels.
Caring for the Spirit: An Illustrative Case
Within the Framework of Systemic Organization, nursing is defined as the process of aiding individuals in achieving harmony both within their own systems and in relation to the broader systems of which they are a part. This concept posits that an individual’s health is intrinsically linked to their alignment with their family, larger societal systems, and the cosmos, making nursing of the family, community, and individual’s spirit an integrated practice.
Spirituality, broadly interpreted, is inherently included in the nursing process, with the framework offering the necessary guidelines to incorporate it effectively. The case of James, a hypothetical figure, serves as a poignant example of this approach.
James, a 69-year-old man with familial responsibilities and a rich personal life, faced involuntary retirement due to a terminal heart disease diagnosis four years prior. This transition profoundly impacted his self-esteem, as the disease stripped him of his traditional role as the family’s breadwinner, leading him to retreat into a life of inactivity, predominantly spent watching television.
Following his diagnosis, James was prescribed a comprehensive treatment plan, including a diet low in sodium and cholesterol, regular exercise, and standard heart medication. However, he resisted these changes, particularly modifying his diet and physical activity.
Initially compliant with his medication regimen, financial constraints soon led him to reduce his intake. Despite encouragement from family and friends to adhere to his treatment plan, James chose to follow his own path, which resulted in the development of diabetes and renal failure.
In the final eight months of his life, James began to release his intense desire for control after realizing his attempts to reclaim his past life were futile. Although he wasn’t ready to face the end of his life, his diminishing physical strength made him more conscious of the need to resolve unfinished matters with his loved ones.
A significant turning point came through his interactions with a visiting male nurse who provided weekly care. Encouraged by the nurse, James opened up about his life, including unresolved grief, feelings of guilt, and particularly an extramarital affair that he had once admitted to his wife but had not been able to fully reconcile.
The act of sharing his guilt and receiving validation from a compassionate professional empowered James to address these feelings with his family. During a family meeting arranged with the nurse’s help, James expressed his remorse for the pain he caused, openly sharing his love for his family. This confession and the family’s acceptance of his apologies allowed James to reconnect with his religious beliefs, finding solace in the anticipation of an afterlife free from suffering. He also chose to sign Advance Directives, enabling him and his family to appreciate their rekindled relationships in his remaining days.
This scenario illustrates the interplay between control and spirituality in nursing care. Throughout most of his life, James prioritized control, with spirituality lying dormant until his circumstances became dire. The supportive relationship with his nurse helped James to see himself as worthy of love, bolstering his self-identity. This newfound self-awareness enabled him to seek deeper connections, starting with his family and extending to his religious faith.
The nurse’s empathetic care facilitated James’s journey towards self-acceptance, allowing him to express his vulnerabilities and ultimately find peace with his family and his spirituality. This process helped James to confront and accept the concept of death, alleviating his fears and providing comfort to his family as they faced the reality of losing him.
Theory of Group Power within Organizations – Christina Sieloff – (our second middle range nursing theory)
Group power is the capacity of a group to fulfill its objectives. Historically, and even in recent times, the concept of power has been perceived in a negative light by many in the nursing profession, including nurse managers and administrators. This perception could stem from the emphasis on the forms of power identified by French and Raven, particularly the use of coercion.
Consequently, nurse managers and administrators might shy away from utilizing power as a tool, thus hindering the effectiveness and efficiency of their nursing teams. This observation is supported by feedback from several chief nurse executives who expressed reluctance to engage in research related to nursing power, citing their disinterest in this type of study.
However, power should be seen as a beneficial asset available to all groups within any healthcare organization. Since every group within a healthcare organization needs to meet its objectives in alignment with the overarching goals of the organization, nurses who overlook the utility of power as a resource are inadvertently restricting their group’s potential to achieve these objectives.
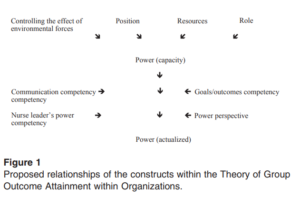
In 1995, Sieloff introduced the middle range nursing theory departmental power during her doctoral studies. Her dissertation work was centered on the initial creation and psychometric evaluation of the instrument related to this theory.
The widespread belief holds that nursing groups play a pivotal role in enhancing patient outcomes and safety, as well as in the financial stability of healthcare organizations. Yet, the exact nature of these contributions by nursing groups has not been thoroughly investigated.
The theory of group outcome attainment within organizations suggests that the degree to which nursing groups achieve outcomes is crucial for: (1) helping patients reach their desired health outcomes, (2) advancing patient safety, and (3) bolstering the financial health of healthcare organizations.
A reliable and valid tool, known as SKAGOAO, has been crafted to assess how nursing groups’ outcome attainment impacts healthcare organizations. This tool is a resource for nurses, managers, educators, and researchers to: (1) highlight the significant contributions of nursing groups to the healthcare setting, and (2) assist nursing groups in devising and executing strategies to enhance their outcome attainment levels.
Implications for Nursing Practice
It is advantageous for all healthcare organizations to acknowledge that nursing groups possess a vital resource: the capability or empowerment to attain outcomes. Familiarizing themselves with this resource allows nursing groups to tap into a potentially underused asset.
Moreover, according to the theory of group outcome attainment within organizations, improving a group’s level of outcome attainment or empowerment is anticipated to lead to better patient outcomes resulting from the nursing group’s interactions with patients.
Implications for Nursing Education
Discussions on power within nursing management and leadership literature often focus on the individual nurse’s capacity to enhance their own power and outcome attainment. Moreover, the perception of power among nurses is not universally positive, as highlighted by the need for this article.
If nursing educators share this ambivalent view, students might graduate without understanding the critical aspect of group outcome attainment. Therefore, it is crucial for nursing education curriculums to incorporate the concept of nursing group outcome attainment or empowerment, particularly within management and leadership courses.
Ideally, this topic should be integrated across all nursing courses to equip nursing groups with the knowledge to enact positive changes in their practice environments.
Implications for Nursing Research
Future applications of the SKAGOAO instrument should include ongoing assessments of its reliability and validity. Ensuring the instrument’s consistency and accuracy is vital for each of its applications, maintaining its integrity. Historically, research has concentrated on individual nurses’ roles within healthcare, with limited attention to the specific contributions of nursing groups.
Employing the SKAGOAO in health services research could both elevate the visibility of nursing groups in healthcare delivery and underscore their essential contributions to patient outcomes, safety, and financial health of healthcare institutions.
Implications for Nursing Management
For nursing management, the SKAGOAO offers valuable insights. Any nursing group, regardless of size, can utilize the SKAGOAO to evaluate their level of outcome attainment or empowerment. This evaluation enables the group to decide whether their current empowerment level is adequate and identify specific areas needing improvement to enhance their empowerment further.
It is essential to recognize that only the group can elevate its empowerment level. Nonetheless, nursing managers and administrators play a crucial role in this process by fostering an environment conducive to nurse participation in decision-making and minimizing overly restrictive controls.
Theory of Comfort – Katharine Kolcaba (our third middle range nursing theory)
Comfort is a fundamental goal in healthcare, essential to the patient’s experience and aimed at achieving a state of well-being. It signifies a positive sensation, embodying satisfaction and bolstering an individual’s resilience in facing crises and difficulties. The improvement in comfort following therapeutic procedures can bolster hope and assurance, aiding in healing, rehabilitation, and the peaceful passing of patients.

Nonetheless, comfort is an intricate notion that challenges definition, measurement, and assessment. Its nature is fleeting and encompasses multiple dimensions, extending beyond merely the absence of pain.
Comfort varies from person to person, characterized by its dynamic quality that can shift within short periods, such as a 20-minute interval. The term “comfort” has diverse interpretations and lacks a universally accepted definition, being used variously as a noun, verb, adjective, and denoting a condition, a progression, and a result. Ongoing research seeks to analyze and understand this concept further.
The absence of a standard definition complicates the measurement of comfort, making it difficult to identify patients’ comfort needs and evaluate the success of interventions aimed at providing comfort. Nurses often face challenges in assessing patients to meet their comfort requirements, highlighting the need for effective, practical, and reliable assessment tools.
Moreover, there is a lack of clarity regarding which interventions are most beneficial for enhancing comfort, and the specific impacts and results of such interventions are infrequently recorded.
Theory of Maternal Role Attainment– Ramona Thieme Mercer (our third middle range nursing theory)
Ramona Thieme Mercer is recognized for her development of the Maternal Role Attainment Theory, a significant contribution to nursing theory that positions her as a notable nurse-theorist. This mid-range theory aims to guide nurses in offering effective health care strategies specifically tailored for non traditional mothers, facilitating their journey towards establishing a robust maternal identity.
The theory is applicable not only during pregnancy and the postpartum period to assist biological mothers in bonding with their newborns but is also valuable for adoptive and foster mothers, or those who assume motherhood roles under unconventional circumstances, such as caring for a child of a relative or friend who has passed away. The essence of the theory lies in fostering a connection between mother and child, which is crucial for the development of a strong mother-child relationship as the infant grows.
At its core, the theory focuses on a developmental and interactive process that unfolds over time, enabling the mother to develop a bond with her child, gain confidence and skill in caregiving tasks, and find fulfillment and happiness in her role as a mother.
The Maternal Role Attainment Theory was created as a guide for nurses to assist nontraditional mothers in forging a strong maternal identity through targeted health care interventions. This theory, applicable both during and after pregnancy, extends its benefits to adoptive or foster mothers and those unexpectedly assuming maternal responsibilities. It emphasizes a process that encourages the formation of a deep bond between mother and infant, fostering a nurturing mother-child relationship as the child matures.
Central to this theory is the idea of a developmental and interactive journey that unfolds over time, allowing the mother to connect with her infant, become proficient in caregiving activities, and ultimately find satisfaction and happiness in being a mother.
The application of the Maternal Role Attainment Theory involves a progression through four distinct stages: anticipatory, formal, informal, and personal. The anticipatory stage involves psychological and social preparation for motherhood, where expectations are formed, and the mother may engage in envisioning her future role.
The formal stage commences with the birth of the child, during which the mother’s actions are often influenced by her social circle and the advice of professionals. The informal stage sees the mother devising and adopting her own caregiving strategies, independent of societal norms or external guidance. Finally, the personal stage is characterized by the mother’s fulfillment and confidence in her maternal role, possibly even contemplating the expansion of her family.
Nurse as Wounded Healer – Marion Conti O’hare (our fourth middle range nursing theory)
When individuals face personal trauma, their coping mechanisms can either succeed or fail. In cases where coping is ineffective, the trauma’s effects go unrecognized, leaving the emotional pain unaddressed. Such individuals often continue their lives as the ‘walking wounded,’ encountering difficulties in social, romantic, and professional relationships. By ignoring their own issues and vulnerabilities, they may inadvertently project their pain onto patients and colleagues, mistakenly believing themselves to be unaffected and showing a reduced capacity for empathy.

Conversely, effective handling of trauma allows the individual to acknowledge and transform the pain into a healing process. Despite the initial harm, the wounds are adequately processed, not hindering the individual’s ability to care for others. This journey of healing turns the individual into a ‘wounded healer,’ capable of using personal experiences of hurt to enhance the care provided to others. Building on this concept, Conti-O’Hare formulated the theory of the nurse as wounded healer, examining how nurses can use their personal adversities to forge stronger therapeutic connections.
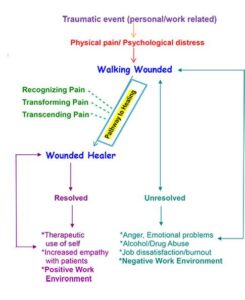
Nurses encounter various traumas that significantly affect both their professional performance and personal lives, influencing the care delivered to patients and the establishment of therapeutic relationships. The Theory of the Nurse as Wounded Healer, a middle-range theory, seeks to identify strategies to mitigate these impacts, enhancing future nursing practice and patient care.
The QUEST model is a tool designed to assist nurses in self-reflection regarding their handling of painful experiences and their journey towards healing. Achieving transformation and transcendence enables nurses to empathize more deeply with patients and colleagues, drawing from their own experiences to facilitate healing and improve patient health and wellbeing.
However, the theory has its limitations, primarily focusing on the healthcare provider’s emotional state and its effect on nursing care delivery. It overlooks the support systems available to nurses from their surroundings, concentrating instead on individual internal battles and the coping strategies employed to surmount them. Additionally, there’s a risk that traumatic experiences might resurface, potentially impacting a nurse’s workplace performance negatively.
Synergy Model – AACN (our fifth middle range nursing theory)
The AACN Synergy Model for Patient Care fundamentally serves as a conceptual framework that matches patient needs with the competencies of nurses. Established in 1996 to innovate AACN’s certification offerings, the Synergy Model transitioned the evaluation of nursing abilities from the traditional body systems/medical model, which often failed to reflect real-world practice, to a focus on “nurse competencies.”
The essence of this model is the premise that the care required by patients dictates the competencies nurses need to possess. When there is a match between the characteristics of the nurse and the needs of the patient, a synergistic relationship is formed, leading to the best possible patient outcomes.
This model outlines eight specific characteristics of patients and eight corresponding nurse competencies, with further details on these aspects provided within the model’s documentation.
Applications of the Synergy Model
Originally designed with a focus on enhancing certification processes within critical care nursing, the creators of the Synergy Model recognized its applicability across a wide range of nursing practices. This is due to the universal relevance of the patient needs identified by the model to all nurse-patient interactions.
Today, the Synergy Model is integral not only to AACN certification processes but also serves as a foundational professional practice model, is incorporated into nursing education curriculums, and supports models for professional development in nursing. Further insights into these applications are elaborated upon in related documentation.
Behavioral Systems Model – Dorothy Johnson (our sixth middle range nursing theory)
The behavioral system model promotes the development of proficient and functional behavior in patients to avert sickness. It conceptualizes the patient as a behavioral system consisting of seven distinct behavioral subsystems: affiliative, dependency, ingestive, eliminative, sexual, aggressive, and achievement-oriented behaviors.
Furthermore, each of these subsystems is governed by three essential functional needs: (1) safeguarding against harmful influences, (2) ensuring a supportive and nurturing environment, and (3) providing stimuli for development and growth. A disruption or imbalance in any of these subsystems leads to a state of disequilibrium. The primary responsibility of the nurse is to assist the patient in restoring and maintaining their balance or equilibrium.
Quality of Nursing care Theory – June H Larrabee (our seventh middle range nursing theory)
In the development of the theory, the concept of value was highlighted through a linguistic analysis aimed at exploring the essence of quality. This analysis delved into the linguistic usage of quality and its associated concepts, revealing that quality possesses both value-laden and value-neutral interpretations.
According to Aristotle, the notion of quality is imbued with value, closely linked to the ideals of excellence and virtue, which are seen as quality’s synonyms. These synonyms underscore the pursuit of desirable characteristics. Larrabee, through this linguistic exploration, deduced that quality signifies a value-rich characteristic suitable for comparative analysis, thereby embedding value as a core element of the Quality of Nursing Care Theory.
Larrabee’s professional experiences further informed this theory, noting that care interventions are often judged by their potential patient benefit. Additionally, there was skepticism about patients’ ability to evaluate and define quality, resulting in patient satisfaction data being overlooked for quality enhancement.
Decisions around quality seldom took into account the costs for patients or society. Traditionally, quality evaluation was confined to areas chosen by healthcare providers or was specific to certain disciplines. In formulating the Quality of Nursing Care Theory, historical and contemporary research on healthcare quality was utilized, where various authors have linked quality with value.
The incorporation of value within a quality framework has received considerable endorsement, as has the inclusion of beneficence or the principle of doing good. However, the integration of prudence and justice within such a framework has seen limited backing.
Theory of Unpleasant Symptoms – Elizabeth R Lenz and Linda C Pugh (our eighth middle range nursing theory)
The Theory of Unpleasant Symptoms stands as a comprehensive mid-range theory that views symptoms through a multidimensional lens. It was conceived based on the understanding that various symptoms exhibit common characteristics, making the theory applicable to a diverse array of symptom types.
This theory delineates four
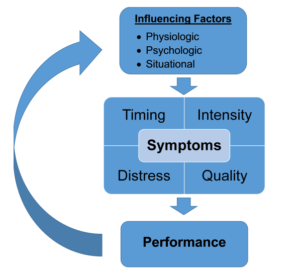
key dimensions of symptoms: their timing, intensity, quality, and the distress they cause, each of which is quantifiable. Factors that might influence the experience of symptoms encompass physiological, psychological, and situational aspects. Additionally, the presence of symptoms can impact key outcomes, affecting behaviors related to seeking care and overall quality of life.
With the evolution of this theory, emphasis has been placed on the potential interplay between different symptoms, where one symptom could potentially trigger another. It also considers how symptoms can influence the factors affecting them through a feedback loop, and how alterations in performance outcomes might reciprocally impact the symptoms and their influencing factors.
This theory effectively captures the intricate and multifaceted nature of experiencing symptoms, acknowledging the myriad variables involved.
